Get approvals quickly
and keep care
moving.
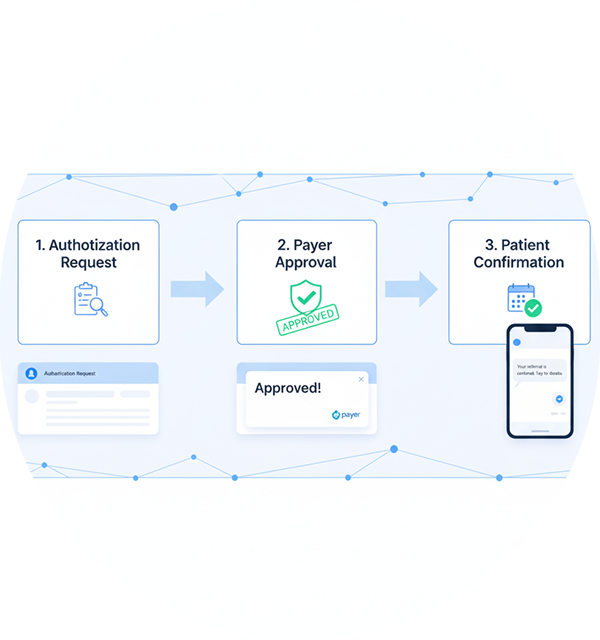
CoordinatorZ manages prior authorizations and
referrals end-to-end, ensuring no delay in patient
care or claim processing. We handle documentation,
tracking, and payer follow-ups with accuracy and
speed.
We help you:
- Prior authorization and referral submission
- Real-time status tracking and escalation
- Documentation management and compliance review